The $2,000 Mistake That Wasn’t Your Fault
Uncover the ways on how medical billing and coding impact your health insurance claims, coverage decisions, and out-of-pocket costs. When David received a staggering bill for his emergency appendectomy, he assumed his insurance had denied the claim. The reality was more frustrating and more common. A coding error had classified his in-network hospital stay as an out-of-network observation visit, triggering higher costs. After six weeks of phone calls between his doctor’s office and insurer, the corrected coding reduced his bill by 80%. This experience reveals what most patients never see: the invisible world of medical billing and coding that quietly determines your healthcare costs and coverage.
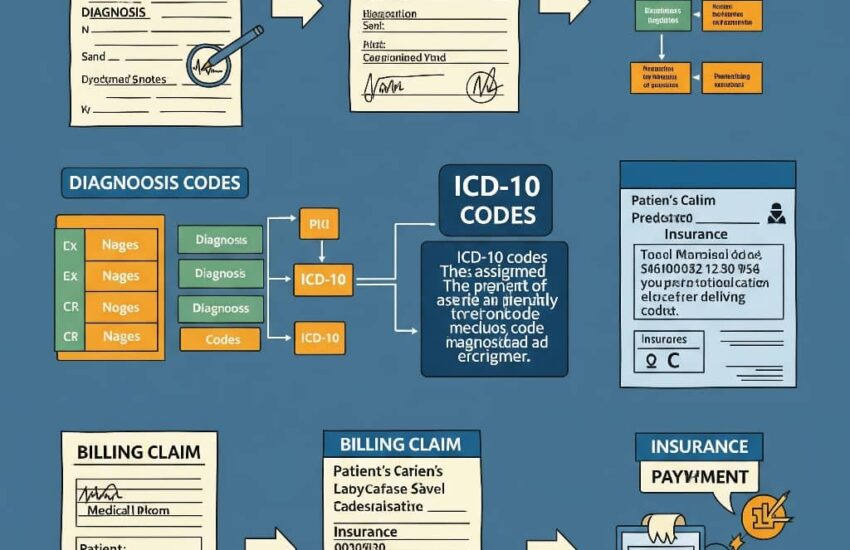
Medical billing and coding form the financial backbone of healthcare, translating services into standardized data that insurers process. When this system works well, claims flow smoothly. When it fails, patients face denied claims, unexpected bills, and hours of frustrating phone calls. Understanding this process helps you navigate coverage challenges more effectively.
How Coding Creates Your Medical Paper Trail
Every healthcare service, from an annual physical to open-heart surgery, gets translated into standardized codes before insurers review it. Coders use two main systems: ICD codes (International Classification of Diseases) for diagnoses and CPT/HCPCS codes (Current Procedural Terminology/Healthcare Common Procedure Coding System) for treatments.
The precision matters tremendously. A routine physical coded as preventive care (CPT 99396) gets fully covered under most plans, while the same visit coded as a problem-focused exam (CPT 99214) might apply to your deductible. Similarly, coding a medication as “experimental” rather than “therapeutic” can mean the difference between coverage and denial.
Specialized coders in your provider’s office review clinical notes to select these codes carefully. However, understaffed offices sometimes rely on overworked coders or automated systems that make mistakes affecting your wallet.
The Billing Process That Determines What You Pay
After coding, your provider’s billing team submits claims to your insurer using electronic forms. Here, three critical factors determine your financial responsibility:
Contractual Agreements: Your insurer has pre-negotiated rates with providers. A $300 test might be “allowed” at $175, with the difference written off.
Benefit Design: Your plan’s rules about deductibles, copays, and coinsurance get applied to the allowed amount.
Claim Scrubbing: Insurers use software to flag discrepancies between codes and medical necessity before paying claims.
Errors at any stage create problems. A physical therapy claim might deny because the coder used a general musculoskeletal code (ICD-10 M25.50) instead of your specific knee pain diagnosis (ICD-10 M25.561). Similarly, bundling separate services incorrectly can make insurers reject claims as “duplicate billing.”
How Patients Can Protect Themselves

While you can’t control the coding process, you can take proactive steps: First, Request detailed itemized bills showing all codes for services, next, you want to compare codes on bills against your explanation of benefits (EOB), Also you can ask providers to resubmit claims with corrected codes when needed and Lastly, Learn basic codes for your frequent services (e.g., diabetes monitoring codes)
Medical billing advocates estimate that up to 80% of medical bills contain errors. One patient saved $1,200 by noticing her MRI was coded as “without contrast” (CPT 70553) when her records showed contrast was used (CPT 70552), changing the coverage determination.
Medical billing and coding function as the silent arbiters of your healthcare coverage, a complex system where numbers and abbreviations determine what services get paid and how much you owe. While the process happens behind the scenes, being informed helps you spot errors, advocate for proper coding, and ultimately ensure your insurance works as intended. When in doubt, remember: the code assigned to your care matters just as much as the care itself in determining your coverage.
References
O’Donnell, S., & Suresh, S. (2022). A systematic review of outpatient billing practices: Importance of accurate medical coding and billing for healthcare reimbursement and compliance. *SAGE Open Medicine*, 10. https://doi.org/10.1177/20503121221099021
American Speech-Language-Hearing Association. (n.d.). Health care billing codes. https://www.asha.org/advocacy/health-care-billing-codes/
University of Houston-Downtown. (n.d.). Medical billing and coding program overview. https://www.uhd.edu/academics/continuing-education/healthcare-programs/health-medicalbilling.aspx
DeVry University. (2023, May 13). Medical billing and coding examples. https://www.devry.edu/blog/examples.html